What is emphysema?
Emphysema is a chronic obstructive pulmonary disease (COPD), formerly termed a chronic obstructive lung disease (COLD). It is often caused by exposure to toxic chemicals, including long-term exposure to tobacco smoke.
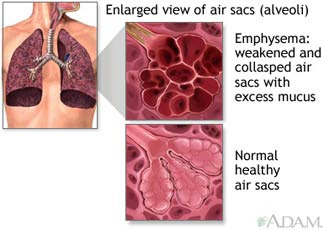
Emphysema is characterized by loss of elasticity (increased Pulmonary compliance) of the lung tissue, from destruction of structures supporting the alveoli, and destruction of capillaries feeding the alveoli, owing to the action of alpha 1 antitrypsin deficiency. Thus the small airways collapse during exhalation, as alveolar collapsibility has increased. This impedes airflow and traps air in the lungs, as with other obstructive lung diseases. Symptoms include shortness of breath on exertion and later at rest, hyperventilation, and an expanded chest.
Mild emphysema sufferers often maintain perfect blood oxygen levels by hyperventilating, and so are sometimes called "pink puffers." By contrast, sufferers of chronic bronchitis (another COPD disorder) are called "blue bloaters" because they have cyanosis (inadequate oxygen) due to an almost normal ventilatory drive caused by decreased sensitivity to carbon dioxide. But any COPD disease results in hypoxaemia (decreased blood partial pressure of oxygen) and hypercapnia (increased blood partial pressure of carbon dioxide).
Signs and Symptoms
Signs of emphysema include pursed-lipped breathing, central cyanosis and finger clubbing. The chest has increased percussion notes, particularly just above the liver, and a difficult to palpate apex beat, both due to hyperinflation. There may be decreased breath sounds and audible expiratory wheeze. In advanced disease, there are signs of fluid overload such as pitting peripheral edema. The face has a ruddy complexion if there is a secondary polycythemia. Sufferers who retain carbon dioxide have asterixis (metabolic flap) at the wrist.
Clinical examination reveals no overt crackles, but in some patients the fine opening of airway 'popping' can be heard. It is unlike the fine crackles of pulmonary fibrosis or coarse crackles of mucus or oedematous fluid.
Emphysema can be cause by the intake or exposure to some toxic chemicals. Another possible cause of emphysema is long term smoking.
Pathophysiology
In normal breathing, air is drawn in through the bronchial passages and down into the increasingly fine network of tubing in the lungs called the alveoli, which are many millions of tiny sacs surrounded by capillaries. These absorb the oxygen and transfer it into the blood. When toxins such as smoke are breathed into the lungs, the particles are trapped and cause a localized inflammatory response. Chemicals released during the inflammatory response (e.g., elastase) can break down the walls of alveoli (alveolar septum). This crucial pathogenic event (septal rupture) leads to significant, purely mechanical modifications of lung architecture, driven by lung elastic recoil which causes parenchyma collapse of the septal rupture confining area and intrapulmonary air collections that exceed the sum of alveoli area made in communication by the septal rupture. As the process proceeds, thoracic cage expansion (barrel chest) and diaphragm contraction (flattening) occur to enhance inspiratory re-expansion/ventilation of the residual partially collapsed healthy parenchyma.Moreover, expiration increasingly depends on the thoracic cage and abdominal muscle action, particularly in the end expiratory phase, instead that on the physiological elastic lung recoil, thus triggering the bronchial obstruction. Mainly decreased is the ability to exude carbon dioxide due to ventilation deficit and, in the more serious cases, oxygen uptake is also impaired. The activity of another molecule called alpha 1-antitrypsin normally neutralizes the destructive action of one of these damaging molecules.
After a prolonged period, hyperventilation becomes inadequate to maintain high enough oxygen levels in the blood. The body compensates by vasoconstricting appropriate vessels. This leads to pulmonary hypertension, which places increased strain on the right side of the heart, the one that pumps deoxygenated blood to the lungs, and it often fails. The failure causes the heart muscle to thicken to pump more blood. This heart condition is often accompanied by the appearance of jugular venous distension. Eventually, as the heart continues to fail, it becomes larger and blood backs up in the liver.
Emphysema occurs in a higher proportion in patients with decreased alpha 1-antitrypsin (A1AT) levels (alpha 1-antitrypsin deficiency, A1AD). In A1AD, inflammatory enzymes (such as elastase) are able to destroy the alveolar tissue (the elastin fibre, for example). Most A1AD patients do not develop clinically significant emphysema, but smoking and severely decreased A1AT levels (10-15%) can cause emphysema at a young age. The pattern of emphysema in A1AD is described as panacinar (involving the entire acinus) as opposed to the centrilobular pattern seen with smoking; the former typically affects the lower lungs, and the latter affects the upper lungs. In all, A1AD causes about 2% of all emphysema. However, smokers with A1AD are in the highest risk category for emphysema.
Pathogenesis
While A1AD provides some insight into the pathogenesis of the disease, hereditary A1AT deficiency only accounts for a small proportion of the disease. Past have focused mainly upon the putative role of leukocyte elastase (also neutrophil elastase), a serine protease found in neutrophils, as a primary contributor to the connective tissue damage seen in the disease. This hypothesis, a result of the observation that neutrophil elastase is the primary substrate for A1AT, and A1AT is the primary inhibitor of neutrophil elastase, together have been known as the "protease-antiprotease" theory, implicating neutrophils as an important mediator of the disease. However, there is a possibility that one of the many other numerous proteases, especially matrix metalloproteases might be equally or more relevant than neutrophil elastase in the development of non-hereditary emphysema.
Research into the pathogenesis of emphysema involved animal experiments where various proteases were instilled into the trachea of various species of animals. These animals developed connective tissue damage, which was taken as support for the protease-antiprotease theory. However, just because these substances can destroy connective tissue in the lung, as anyone would be able to predict, doesn't establish causality. More recent experiments have focused on more technologically advanced approaches, such as ones involving genetic manipulation. Perhaps the most interesting development with respect to our understanding of the disease involves the production of protease "knock-out" animals, which are genetically deficient in one or more protease.
Associations
Emphysema is commonly associated with bronchitis and chronic bronchitis. Since it is difficult to delineate "pure" cases of emphysema or chronic bronchitis, they are generally grouped together as chronic obstructive pulmonary disease (COPD).
Severe cases of A1AD may also develop cirrhosis of the liver, where the accumulated A1AT leads to a fibrotic reaction.
Emphysema can be classified into two types: Primary and Secondary. Primary emphysema can be subdivided into panacinary and centroacinary. Panacinary emphysema is related to the destruction of alveoli, because of an inflammation or deficiency of alfa-1-antitrypsin. It is found more in young adults who do not have chronic bronchitis. Centroacinary emphysema is due to destruction of terminal bronchioli muchosis, due to chronic bronchitis. This is found mostly in elderly people with a long history of smoking.
Treatment
Emphysema is an irreversible degenerative condition. The most important measure to slow its progression is for the patient to stop smoking and avoid all exposure to cigarette smoke and lung irritants. Pulmonary rehabilitation can be very helpful to optimize the patient's quality of life and teach the patient how to actively manage his or her care.
Emphysema is also treated by supporting the breathing with anticholinergics, bronchodilators, steroid medication (inhaled or oral), and supplemental oxygen as required. Treating the patient's other conditions including gastric reflux and allergies may improve lung function. Supplemental oxygen used as prescribed (usually more than 20 hours per day) is the only non-surgical treatment which has been shown to prolong life in emphysema patients. There are lightweight portable oxygen systems which allow patients increased mobility. Patients can fly, cruise, and work while using supplemental oxygen. Other medications are being researched.
Lung volume reduction surgery (LVRS) can improve the quality of life for certain carefully selected patients. It can be done by different methods, some of which are minimally invasive. In July 2006 a new treatment, placing tiny valves in passages leading to diseased lung areas, was announced to have good results, but 7% of patients suffered partial lung collapse. The only known "cure" for emphysema is lung transplant, but few patients are strong enough physically to survive the surgery. The combination of a patient's age, oxygen deprivation and the side-effects of the medications used to treat emphysema cause damage to the kidneys, heart and other organs. Transplants also require the patient to take an anti-rejection drug regime which suppresses the immune system, and so can lead to microbial infection of the patient.














No comments:
Post a Comment