
The pancreas is a gland organ in the digestive and endocrine system of vertebrates. It is both an endocrine gland (producing several important hormones, including insulin, glucagon, and somatostatin), as well as an exocrine gland, secreting pancreatic juice containing digestive enzymes that pass to the small intestine. These enzymes help in the further breakdown of the carbohydrates, protein, and fat in the chyme.

Histology
Under a microscope, stained sections of the pancreas reveal two different types of parenchymal tissue. Lightly staining clusters of cells are called islets of Langerhans, which produce hormones that underlie the endocrine functions of the pancreas. Darker staining cells form acini connected to ducts. Acinar cells belong to the exocrine pancreas and secrete digestive enzymes into the gut via a system of ducts.
Function
The pancreas is a dual-function gland, having features o
f both endocrine and exocrine glands.
Endocrine
The part of the pancreas with endocrine function is made up of a million cell clusters called islets of Langerhans. There are four main cell types in the islets. They are relatively difficult to distinguish using standard staining techniques, but they can be classified by their secretion: α cells secrete glucagon, β cells secrete insulin, δ cells secrete somatostatin, and PP cells secrete pancreatic polypeptide.
The islets are a compact collection of endocrine cells arranged in clusters and cords and are crisscrossed by a dense network of capillaries. The capillaries of the islets are lined by layers of endocrine cells in direct contact with vessels, and most endocrine cells are in direct contact with blood vessels, by either cytoplasmic processes or by direct apposition. According to the volume The Body, by Alan E. Nourse, the islets are "busily manufacturing their hormone and generally disregarding the pancreatic cells all around them, as though they were located in some completely different part of the body."
Exocrine
In contrast to the endocrine pancreas, which secretes hormones into the blood, the exocrine pancreas produces digestive enzymes and an alkaline fluid, and secretes them into the small intestine through a system of exocrine ducts in response to the small intestine hormones secretin and cholecystokinin. Digestive enzymes include trypsin, chymotrypsin, pancreatic lipase, and pancreatic amylase, and are produced and secreted by acinar cells of the exocrine pancreas. Specific cells that line the pancreatic ducts, called centroacinar cells, secrete a bicarbonate- and salt-rich solution into the small intestine.
Regulation
The pancreas receives regulatory innervation via hormones in the blood and through the autonomic nervous system. These two inputs regulate the secretory activity of the pancreas.
Diseases of the pancreas
Because the pancreas is a storage depot for digestive enzymes, injury to the pancreas is potentially very dangerous. A puncture of the pancreas generally requires prompt and experienced medical intervention.
History
The pancreas was first identified by Herophilus (335-280 BC), a Greek anatomist and surgeon. Only a few hundred years later, Ruphos, another Greek anatomist, gave the pancreas its name.
Embryological development
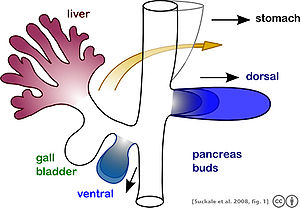
The pancreas forms from the embryonic foregut and is therefore of endodermal origin. Pancreatic development begins the formation of a ventral and dorsal anlage (or buds). Each structure communicates with the foregut through a duct. The ventral pancreatic bud becomes the head and unciate process, and comes from the hepatic diverticulum.
Differential rotation and fusion of the ventral and dorsal pancreatic buds results in the formation of the definitive pancreas. As the duodenum rotates to the right, it carries with it the ventral pancreatic bud and common bile duct. Upon reaching its final destination, the ventral pancreatic bud fuses with the much larger dorsal pancreatic bud. At this point of fusion, the main ducts of the ventral and dorsal pancreatic buds fuse, forming the duct of Wirsung, the main pancreatic duct.
Differentiation of cells of the pancreas proceeds through two different pathways, corresponding to the dual endocrine and exocrine functions of the pancreas. In progenitor cells of the exocrine pancreas, important molecules that induce differentiation include follistatin, fibroblast growth factors, and activation of the Notch receptor system. Development of the exocrine acini progresses through three successive stages. These include the predifferentiated, protodifferentiated, and differentiated stages, which correspond to undetectable, low, and high levels of digestive enzyme activity, respectively.
Progenitor cells of the endocrine pancreas arise from cells of the protodifferentiated stage of the exocrine pancreas. Under the influence of neurogenin-3 and Isl-1, but in the absence of Notch receptor signaling, these cells differentiate to form two lines of committed endocrine precursor cells. The first line, under the direction of Pax-6, forms α- and γ- cells, which produce the peptides glucagon and pancreatic polypeptide, respectively. The second line, influenced by Pax-4, produces β- and δ-cells, which secrete insulin and somatostatin, respectively.
Insulin and glucagon can be detected in the fetal circulation by the fourth or fifth month of fetal development.












No comments:
Post a Comment